Biofilm as a SARS-CoV-2 Virus Reservoir for Fomite Transmission, the WHO’s 5th Category
by N. Stephenson & W. Battistutti
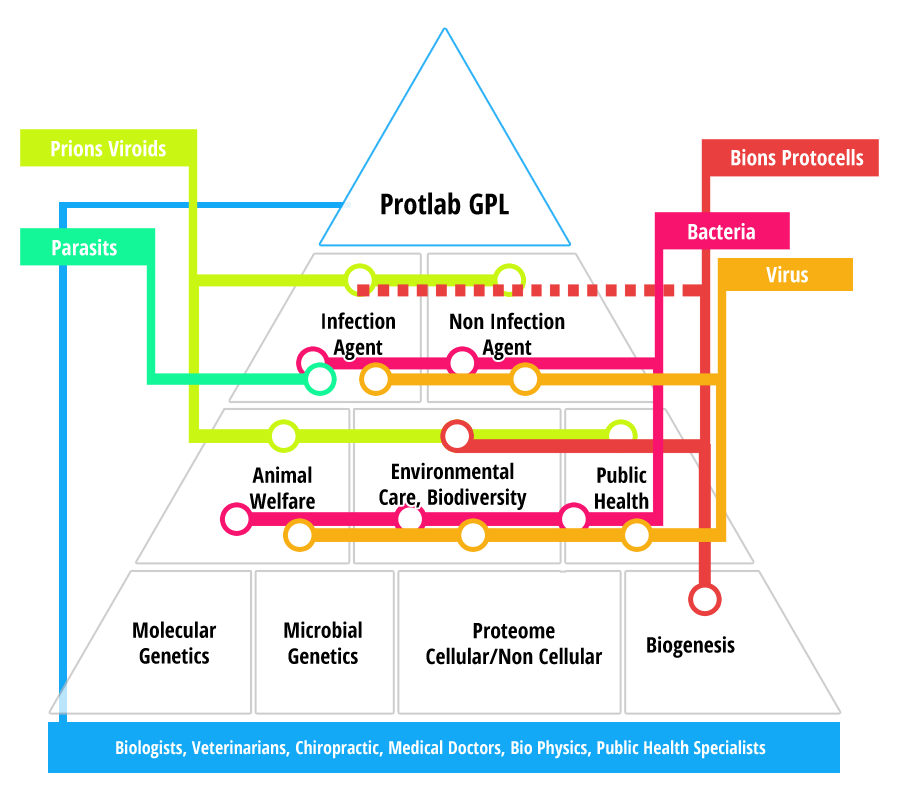
Protlab GPL’s editorial response to the transmission categories reported on in the WHO global study of origins.
The WHO COVID-19 Origins of Sars Study of the 30th March 2021 identified ‘possible pathways of emergence’ in a 120 page report focusing on four categories of transmission:
- direct zoonotic transmission (also termed: spillover)
- introduction through an intermediate host followed by zoonotic transmission
- introduction through the cold/ food chain
- and introduction through a laboratory incident [1].
The result was that there was no conclusive evidence that the origin was wholly attributable to zoonotic transmission or that it originated from the Huanan market or Wuhan laboratory.
Genomic and proteomic analysis of the SARS-CoV-2 virus has identified markers that relate to bat species as well as both pangolin and farmed mink. ‘However, the presence of SARS-CoV-2 has not been detected through sampling and testing of bats or of wildlife across China. More than 80 000 wildlife, livestock and poultry samples were collected from 31 provinces in China and no positive result was identified for SARS-CoV-2 antibody or nucleic acid before and after the SARS-CoV-2 outbreak in China. Through extensive testing of animal products in the Huanan market, no evidence of animal infections was found’ [1].
As such, the report concluded that there is uncertainty of direct or intermediate animal to human transmission and little linked to ingestion of infected meat, in addition testing found no evidence that the pathway to emergence was from the Wuhan laboratory. The lack of certain direct transmission indicates that there are other active ingredients at play, as does the findings that ‘the closest genetic relationship with SARS-CoV-2 was a bat virus, more detailed analysis found evidence for several decades of evolutionary space between the viruses’ [1], the ‘ decades of evolution’ being speculative.
In July 2020, WHO issued a scientific brief that outlined a fifth category of transmission that was not addressed in the ‘Global origins of Sars’ report, that of ’Fomite transmission’. ‘Respiratory secretions or droplets expelled by infected individuals can contaminate surfaces and objects, creating fomites (contaminated surfaces). Viable SARS-CoV-2 virus and/or RNA detected by RT-PCR can be found on those surfaces for periods ranging from hours to days, depending on the ambient environment (including temperature and humidity) and the type of surface’ [2].
Despite there not being extensive research into ‘fomite transmission’ causality, the report did acknowledge that ‘Environmental sampling in Huanan market from right at the point of its closing showed out of 923 environmental samples in Huanan market, 73 samples were positive. This revealed widespread contamination of surfaces with SARS-CoV-2, compatible with introduction of the virus through infected people, infected animals or contaminated products’ [1].
The July 2020, the scientific brief also highlighted that ‘fomite transmission is considered a likely mode of transmission for SARS-CoV-2, given consistent findings about environmental contamination in the vicinity of infected cases and the fact that other coronaviruses and respiratory viruses can transmit this way’ [2].
The Oxford dictionary defines the term ‘fomite’ as ‘Objects or materials which are likely to carry infection, such as clothes, utensils, and furniture’, however, the brief does not explain why viable SARS-CoV-2 virus and/or RNA can survive for days as opposed to minutes in aerosol form. ‘Ong et al. studied several samples taken from the furniture and fixtures from an infected patient’s room (before routine cleaning of the room). Interestingly, all the samples returned positive for the virus’ [3]. ‘Work by Doremalen et al. demonstrated that aerosolized SARS-CoV-2 remains viable in the aerosols for 3 h and on different surfaces for 4–72 h’ [4]. Infectious aerosol droplets that do survive, fall onto surfaces and adhere to other organisms on surfaces and some are absorbed into or form biofilms.
‘A common misconception of microbial living is that bacteria exist as individual organisms in a ‘planktonic state’. Rather, microorganisms have been shown to naturally accumulate on a wide variety of surfaces; where they form sessile, sedentary communities ………. These accumulations of microorganisms of mono- or poly-microbial aggregates are commonly referred to as a biofilm and can consist of diverse communities including other bacteria, fungi, algae and particulate matter [5]. This initial attachment is the first stage of the life cycle of a biofilm. These ‘colonies’ of microorganisms interact, forming ‘a protective layer of extracellular polysaccharides, structural proteins, cell debris and nucleic acids; referred to as extracellular polymeric substances (EPS)’ [5] that extends the viability of the virus by days and provides an environment that enables the substrate interaction between organisms in the maturation stage.
‘An established biofilm structure comprises microbial cells and EPS, has a defined architecture, and provides an optimal environment for the exchange of genetic material. Nucleic acid particles may also communicate via quorum sensing, which may in turn affect biofilm processes such as detachment’ [6]. Biofilms can be detached through touch, however, they also eventually reach optimum growth and naturally expel potentially more virulent mutated viruses back into the air for us to breathe in the dispersion stage. ‘Like all sessile organisms, surface-attached communities of microorganisms known as biofilms must release and disperse genetic material into the environment to colonize new sites. For many pathogenic biofilms, dispersal plays an important role in the transmission from environmental reservoirs to human hosts’ [7].
‘Biofilm infections are estimated to be responsible for up to 80% of all infections in humans and animals, posing a major health challenge (Microbiology Society, 2019)’ [8]. ‘Modelling the weekly death rate in the UK, a maximum-likelihood analysis finds a statistically significant fomite contribution, with 0.009 ± 0.001 (95% CI) infection-inducing fomites introduced into the environment per day per infectious person …… suggests fomites, through enhancing the overall transmission rate, may have contributed to as much as 25% of the deaths following lockdown’ [9].
So there is a reasonable argument to suggest a possible scenario that the SARS-CoV-2 virus could have been hosted and transported by biofilm acting as a catalyst to the evolution of the virus through the bonding of micro-organisms and in turn, becoming the disease vector of famine transmission.
The 2003 SARS outbreak in China was not too distant and ‘there was evidence for supply chains leading to wild-life farms from provinces where the higher prevalence of SARSr-CoVs have been detected in bat surveys’ [1]. The outbreak of SARS-CoV2 in a highly industrialized region can be explained with Biofilm systems development, which appear ideal for the degradation of xenobiotics because of the many reported advantages they have over planktonic cultures (10).
The SARS-CoV-2 viral genome has been proven to be very adaptable and to have a proclivity to mutate and as such is not a single entity. The original virulent material might have come from bats which was deposited on a surface, forming or adhering to an existing biofilm colony and merging with other mutagens and even pathogenic human material which would facilitate quicker, more effective transmission. ‘the optimal environment for virus adaptation is provided by the hosts with intermediate levels of immunity. This is because such individuals represent an appropriate environment for the optimization of both the pathogen population size and the strength of the immune-mediated selection. All the accumulated data indicate that SARS-CoV-2 may gain some adaptation and enhanced virulence, globally contributing to its pathogenicity and transmission’ [11].
Identifying the ‘active ingredients’ of the root source or cocktail of sources would certainly benefit future planning so that mitigation measures can be put in place to prevent future outbreaks and considerable research has been done, though it’s not clear whether surface material sampling was done in the immediate timeline of the current pandemic. Surface-associated behaviors such as biofilm formation and swarming motility allow microbes to establish communities with enhanced protection against external agonists and promote colonization and penetration of biotic and abiotic surfaces[12,13].
The WHO report provided evidence that ‘SARS-CoV-2 has been identified in an increasing number of animal species, but genetic and epidemiological studies have suggested that these were infections introduced from humans, rather than enzootic virus circulation’ [1]. It has to be emphasised that viruses are not transmitted only from animal to man, but evolve in any environment they pass through, ‘An important feature of SARS-CoV-2 is the ability of this virus to be transmitted from human to household pets’ [11].
Further research is needed to identify the active ingredients of micro-organisms that combine to form the many variants that evolve. This includes, both animal and human pathogenic material, proteins and genes, as well as environmental micro-organisms and particulate matter. The human immune system is less efficient as other animals and can harbour a considerable number of virulent organisms that can influence the pathogenesis of virus mutations/variants. For example, Rickettsia tsutsugamushi – As an interesting note, prior infection by Orientia tsutsugamushi has been reported to retard the progression of HIV infection (in terms of viral load). It seems that the HIV virus shares homologous genes with Orientia tsutsugamushi and antigens coded by these genes elicit antibodies that are somewhat protective against the virus. The Alpha Proteobacteria in general are characterized by their small size, and their intimate associations with eukaryotic cells. The Alpha Proteobacteria live as symbionts, as endosymbionts, or as intracellular parasites – same like viruses[14].
As the WHO emphasises, there has to be further research done to identify potential reservoir hosts, however, extensive WHO research has not identified any single indigenous host that would account for the virus, let alone the numerous variants/mutations. Whatever the origin of the nucleotide sequence of this virus was, it needed the support from a biofilm environment which developed into a human pathogenic biofilm (hpb). This hpb could have travelled from areas identified by WHO, remained viable for several days and initiated the outbreak, ‘evidence for supply chains leading to wild-life farms from provinces where the higher prevalence of SARSr-CoVs have been detected in bat surveys’ [1].
Biofilm can be found on all types of surface/fomites, including food and even ice from contaminated water sources and can either be inhaled from aerosol disbursement of mature biofilm or be picked up by man’s propensity to touch and be ingested or to enter the bloodstream ‘available data indicate that the oral cavity may be an active site of infection and an important reservoir of SARS-CoV-2 ……. oral species have been found in the lung of COVID-19 patients. [15]. The oral cavity is proven to be a primary access point for infections.
Profiling can isolate active ingredients that colonise sampled biofilms to help identify the equations that evolve into virulent infectious disease, including SARS-CoV-2. Social interactions among microbes give rise to multicellular groups having emergent behaviours that are not possible in single cells, ‘quorum sensing enables synchronization of gene expression and cellular activities to allow a population to act as a group’ [16,17].
It is important to note that infectious and parasitic diseases for example are interconnected. Those caused by viruses, such as COVID-19, strongly interfere with the immune system, at least via what is being called as a “cytokine storm,” which creates ideal conditions for other co- infections, caused by fungi, protozoa, and helminths, to appear. Little is known about biofilm and their residents, but we know that viruses also infect protozoa, fungi, helminths, and insects that transmit various parasitic protozoa, in addition to interfering with their biological properties. As far as protozoa are concerned, it is worth remembering that in the 1960s, electron microscopy began to show the presence of viral particles in several members of the trypanosomatidae family, in giardia, trichomonas, and cryptosporidium, among others. Identification of the “inhabitants” of biofilm formation should be expanded based on the considerable multi-disciplinary scientific research and publications.‘In extreme cases, multispecies biofilms and microbial mats constitute complex microbial ecosystems where numerous microbes communicate, cooperate and battle with each other’ [18].
Ultimately, the goal of the genome is to enhance its survival and the proliferation of the organism and when the microbe is a pathogen, this has dire consequences for the host. ‘In the biofilm world, cell-cell communication is the rule and considering social behavior as a ubiquitous property of bacteria has transformed our view and understanding of microbiology’ [19,20].
Biofilm should be taken seriously as a transmission category. Biofilms are potentially environmental reservoirs for SARS-CoV-2, acting as carriers on fomites, extending the viable life-span, forming more virulent strains, disbursing the virus back into an aerosol and being directly ingested. Social behaviours are also well-documented in eukaryotic microbes, however, despite the tremendous influence that the paradigm of “socio-microbiology” has had on our understanding of microbiology in biofilm formation, one group of microbes, the parasitic protozoa, seem to have been left without an invitation to the party. Studies of these organisms generally consider them as individual cells in suspension cultures or animal models of infection, while social interactions are largely unstudied. Furthermore, with this group there are also viruses on the banquet of biofilm formations as a lot of parasitic protozoa are transmitters of viral infection disease.
Parasitic protozoa are etiologic agents of several major human maladies, including malaria, epidemic dysentery, leishmaniasis and African sleeping sickness, that affect over half a billion people worldwide. To create an epidemic precondition, multispecies biofilm formations of bacteria, viruses, e.g. partitiviruses and chrysoviruses primarily infect prokaryotes and primitive eukaryotes, such as protozoa and fungi exchanging cell-cell signalling and cell density dependent behaviour, creating, with the assistance of man’s environment, the perfect condition for a successful life on a surface, to conquer the globe.
References:
- WHO-convened global study of origins of SARS-CoV-2: China Part Joint WHO-China study: 30 March 2021 | COVID-19: Animal-human interface and food safety hSps://www.who.int/publications/i/item/who-convened-global-study-of-origins-of- sars-cov-2-china-part
- Organisation W.H.O. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations 2020. https://www.who.int/news- room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19- implications-for-ipc-precaution-recommendations
- Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323816:1610–1612. doi: 10.1001/jama.2020.3227. Recognition of aerosol transmission of infectious agents: a commentary | BMC Infectious Diseases | Full Text (biomedcentral.com)
- Karia R, Gupta I, Khandait H, Yadav A, Yadav A. COVID-19 and its Modes of Transmission. SN Compr Clin Med. 2020 Sep 1:1-4. doi: 10.1007/s42399-020-00498-4. Epub ahead of print. PMID: 32904860; PMCID: PMC7461745. COVID-19 and its Modes of Transmission (nih.gov)
- Birte Hollmann, Mark Perkins, Dean Walsh. Centre of Biomolecular Sciences, University of Nottingham. Biofilms and their role in pathogenesis. Published by the British Society for Immunology
- Donlan RM. Biofilms: microbial life on surfaces. Emerg Infect Dis. 2002 Sep;8(9):881-90. doi: 10.3201/eid0809.020063. PMID: 12194761; PMCID: PMC2732559. Biofilms: Microbial Life on Surfaces (nih.gov)
- Kaplan JB. Biofilm dispersal: mechanisms, clinical implications, and potential therapeutic uses. J Dent Res. 2010 Mar;89(3):205-18. doi: 10.1177/0022034509359403. Epub 2010 Feb 5. PMID: 20139339; PMCID: PMC3318030. Biofilm Dispersal (nih.gov)
- https://www.biofilms.ac.uk/
- Meiksin A. Dynamics of COVID-19 transmission including indirect transmission mechanisms: a mathematical analysis. Epidemiol Infect. 2020 Oct 23;148:e257. doi: 10.1017/S0950268820002563. PMID: 33092672; PMCID: PMC7642914. Dynamics of COVID-19 transmission including indirect transmission mechanisms: a mathemaMcal analysis (nih.gov)
- Barry Heffernan, Cormac D. Murphy, and Eoin Casey. Comparison of Planktonic and Biofilm Cultures of Pseudomonas fluorescens DSM 8341 Cells Grown on Fluoroacetate (Applied and Environmental Microbiology, 17Dec2020) https://doi.org/ 10.1128/AEM.01530-08
- Elrashdy F, Redwan EM, Uversky VN. Why COVID-19 Transmission Is More Efficient and Aggressive Than Viral Transmission in Previous Coronavirus Epidemics? Biomolecules. 2020 Sep 11;10(9):1312. doi: 10.3390/biom10091312. PMID: 32933047; PMCID: PMC7565143. Biomolecules | Free Full-Text | Why COVID-19 Transmission Is More Efficient and Aggressive Than Viral Transmission in Previous Coronavirus Epidemics? | HTML (mdpi.com)
- Bassler B, Losick R. Bacterially Speaking. Cell. 2006;125:237–246. An excellent review that describes communication systems used by bacteria, including long and short range signaling systems, as well as examples of multicellular community development and fratricide. https://doi.org/10.1016/j.cell.2006.04.001
- Shapiro JA. Thinking about bacterial populations as multicellular organisms. Annu Rev Microbiol. 1998;52:81–104. This review discusses the concepts of social behavior in bacteria and the impact that considering bacteria as social organisms has had on our view of microbiology. DOI: 10.1146/annurev.micro.52.1.81
- Parsek MR, Greenberg EP. Sociomicrobiology: the connecMons between quorum sensing and biofilms. Trends Microbiol. 2005;13:27–33. This review introduces the term “sociomicrobiology” and considers the impact of social interactions on microbes and microbial pathogenesis. DOI: 10.1016/j.tim.2004.11.007
- Xiang Z, Koo H, Chen Q, Zhou X, Liu Y, Simon-Soro A. Potential implications of SARS-CoV-2 oral infection in the host microbiota. J Oral Microbiol. 2020 Nov 29;13(1):1853451. doi:10.1080/20002297.2020.1853451. PMID: 33312449; PMCID: PMC7711743. Potential implications of SARS-CoV-2 oral infection in the host microbiota (nih.gov)
- Jules J. German , Taxonomic Guide to Infectious Diseases (Second Edition), 2019 – SecMon 3.2 AlphaProteobacteria Paperback ISBN:9780128175767
- Pacheco AR, Sperandio V. Inter-kingdom signaling: chemical language between bacteria and host. Curr Opin Microbiol. 2009;12:192–198. DOI: 10.1016/ j.mib.2009.01.006
- Bassler B, Losick R. Bacterially Speaking. Cell. 2006;125:237–246. An excellent review that describes communication systems used by bacteria, including long and short range signaling systems, as well as examples of multicellular community development and fratricide. https://doi.org/10.1016/j.cell.2006.04.001
- Verstrepen KJ, Fink GR. Genetic and epigenetic mechanisms underlying cell- surface variability in protozoa and fungi. Annual Review of Genetics. 2009;43:1 DOI: 10.1146/annurev-genet-102108-134156
- Plant virus interacMon in nitrogen-fixing nodules (Journal of plant diseases and protecMon, Vol.91,No 2 April 1984, pp200-212